https://unbfpsyc.ca1.qualtrics.com/jfe/form/SV_3QU7KNgS3G0aPHw
Not All Catheter Coatings Are the Same

The truth is . . . intermittent catheterization can add up
Intermittent catheterization (IC) can add up – catheterizing 6 times every day equals 2,190 catheterizations each year. This can add up financially too; balancing the financial burden and frequency of catheterization leads many Canadians to re-use single-use catheters.
Canadian clinicians recommend single-use
As of 2020, Canadian urologists and nurses recommend single use intermittent catheters, ideally those that are hydrophilic or pre-lubricated.1,2 In fact, Canadian nurses no longer support the re-use of intermittent catheters at all.1

Why single use?
Re-using catheters can also be inconvenient and cumbersome. Having to spend time washing, sanitizing, drying and storing your catheters only makes your bladder management routine longer. Re-using catheters also adds extra steps when you prepare to leave the house. Whether it is to go to work, go shopping, or visit loved ones, having to pack supplies to wash, sanitize and store used catheters can be an inconvenience. Having a catheterization routine that you find convenient and are satisfied with can help you stick to your schedule and empty your bladder as recommended by your doctor3, which supports your bladder health. 4,5,6
Finally, and perhaps most importantly, re-using catheters may lead to a change of physical properties of the catheter material and there is a risk of introducing harmful bacteria, which may result in a urinary tract infection (UTI).7,8
You may already be covered
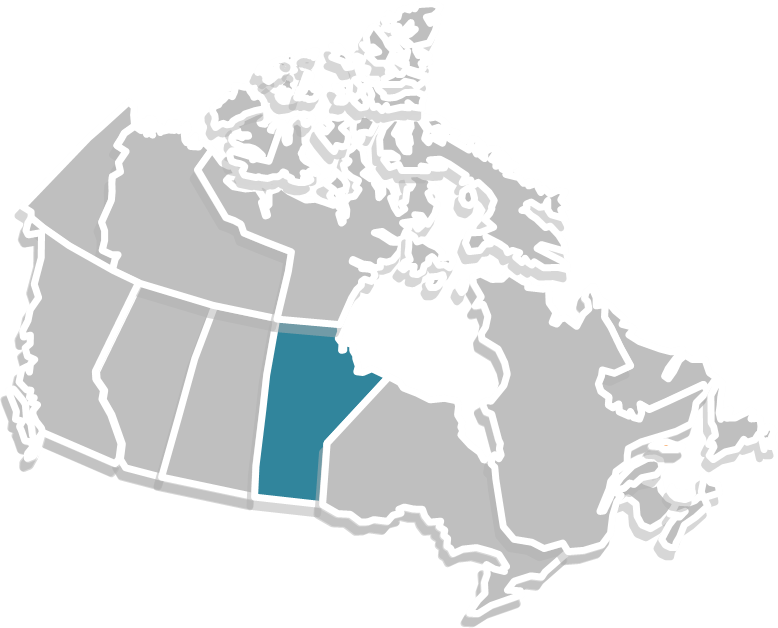
Product reimbursement in Canada can be complex and overwhelming. You may not be aware that your private insurance or provincial support covers catheters or that you may even qualify for a hydrophilic or compact solution. In Manitoba, possible funding options can include Employment and Income Assistance (EIA), Worker Compensation Board of Manitoba (WCB Manitoba), Non-Insured Health Benefits (NIHB), Jordan’s Principle (developed and made available by Assembly of First Nations), Public Service Health Care plan, and Veterans Affairs Canada (VAC), as well as possible municipal programs and Canada tax credit/financial support programs. Private coverage is another option and many benefit plans offer better catheter coverage than you may think. Often, all you need is a prescription, or Letter of Recommendation from your doctor. The Coloplast Letter of Recommendation can provide additional support for your claim, by giving providers a rationale as to why you need a specific catheter. The Coloplast Letter of Recommendation has successfully helped Canadian catheter users access reimbursement for their intermittent catheters.
- Clean Intermittent Urethral Catheterization in Adults – Canadian Best Practice Recommendations for Nurses. Developed by Nurses Specialized in Wound, Ostomy and Continence Canada, Canadian Nurse Continence Advisors, Urology Nurses of Canada, and Infection Prevention and Control.1st Ed. 2020.
- Can Urol Assoc J 2020;14(7):E281-9. http://dx.doi.org/10.5489/cuaj.6697
- Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance and per- sistence. Patient Preference and Adherence. 2012; 6: 39–48
- Wyndaele JJ. Complications of intermittent catheterization: their prevention and treatment. Spinal Cord. 2002; 40(10): 536-41.
- Neal DE, Lawson AL, Webb RJ, Robertson AS. Clean intermittent self-catheterization. Int Urogynecology J. 1993; 4(1): 50-5.
- Grabe M, et al. Guidelines on Urological Infections. European Association of Urology. 2012; 28.
- Bogaert GA, Goeman L, de Ridder D, Wevers M, Ivens J, Schuermans A. The physical and antimicrobial effects of microwave heating and alcohol immersion on cathe- ters that are reused for clean intermittent catheterisartion. Eur Urol. 2004;46(5):641-6
- Chan JL, Cooney TE, Schober JM. Adequacy of sanitization and storage of catheters for intermittent use after washing and microwave sterilization. J Urol. 2009;182(4 Suppl):2085-9

